There have always been very few dedicated tools and techniques for restoratively-driven papilla regeneration. And traditional approaches to direct composites are known to significantly compromise the patient’s periodontal health.
This was, until, the development of the Bioclear Matrix System, which takes a non-invasive and predictable approach to restorative dentistry.
 To truly grasp an understanding of what has changed when it comes to treating black triangles, we take a closer look at the conventional treatment options available and the advancement that has transformed direct composites.
To truly grasp an understanding of what has changed when it comes to treating black triangles, we take a closer look at the conventional treatment options available and the advancement that has transformed direct composites.
Traditional Treatment Options: Loss Of Interdental Papilla
Before the introduction of the Bioclear Method, dentists had three main treatment modalities to choose from:
1. Orthodontic Treatment or Re-treatment
Typically undertaken to correct overcrowding, adult orthodontic treatment can be extremely effective at improving the aesthetics of tooth position. However, this solution often blunts the papillae and can lead to black triangles.
When a patient presented with this problem, it was very common for clinicians to retreat them orthodontically:
- The affected teeth would be aggressively stripped in the interproximal areas, with lightning strips or a high-speed handpiece and diamond burs.
- The dental arches would then be ‘collapsed’ to approximate the roots, compressing the interdental papillae.
- The papillae would then gradually swell incisally and engage the contact area.
However, as well as being both expensive and time consuming, this method can often compromise tooth position and arch size.
Prosthetic Intervention
Although porcelain laminate veneers, or full-coverage porcelain crowns, have been proved as a successful treatment option, they do come with some a significant risk of actually worsening the appearance of black triangles.
This is down to the act of tissue retrations, combined with the negative effects of the interim prosthesis. There is also the potential of unsightly cyanotic and engorged tissues.
Microsurgical Papilla Regeneration Procedures
Recognised as an ‘exotic’ procedure, microsurgical papilla regeneration procedures have proven to be an effective solution to black triangles. However, this nuanced procedure is beyond the scope of most general and periodontal speciality practices, making it an inaccessible solution for most.
So what does this mean for dentists?
It’s no surprise that many dental professionals have been inclined to ignore this problem. This is because traditional methods available fail to offer reliable and predictable solutions that are both cost effective and minimally invasive.
In 2009, Dr Clark invented Bioclear - a non-invasive, additive method which makes a direct restorative solution to black triangles both simple and predictable.
Here it is, in action:










A Suitable Candidate For Papilla Regeneration
Any restorative procedure involving the interproximal area is a candidate for papilla regeneration.
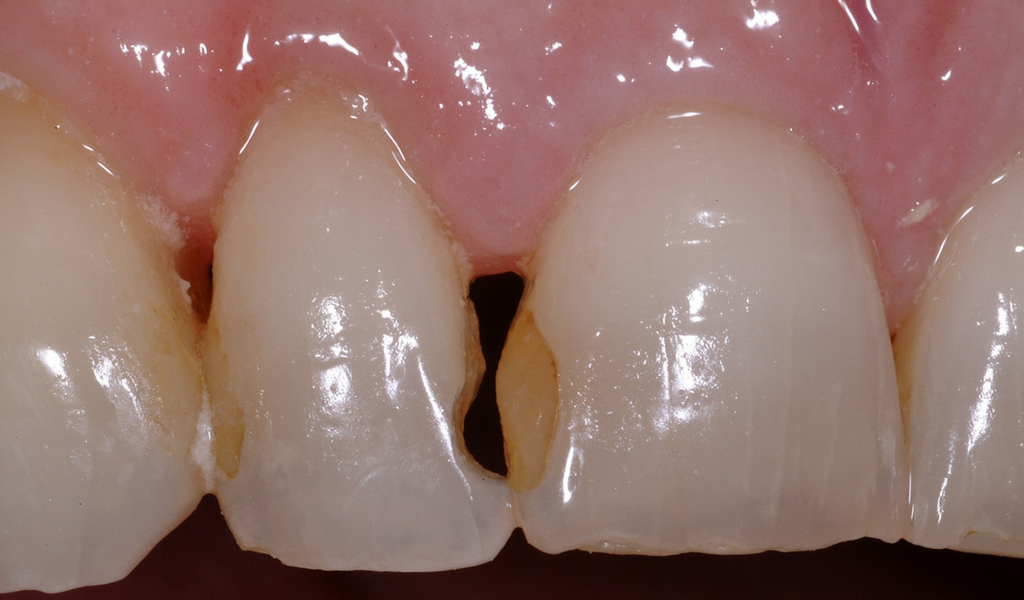
This clinical case begins as a restorative treatment; the patient originally presented with failing silicate restorations on the mesial of the upper right lateral incisor, and the distal of the right central incisor. They also had blunted papilla, or ‘black triangles’.
In the first instance, they only wanted the interproximal area to be treated.
Black Triangle Treatment: Step 1
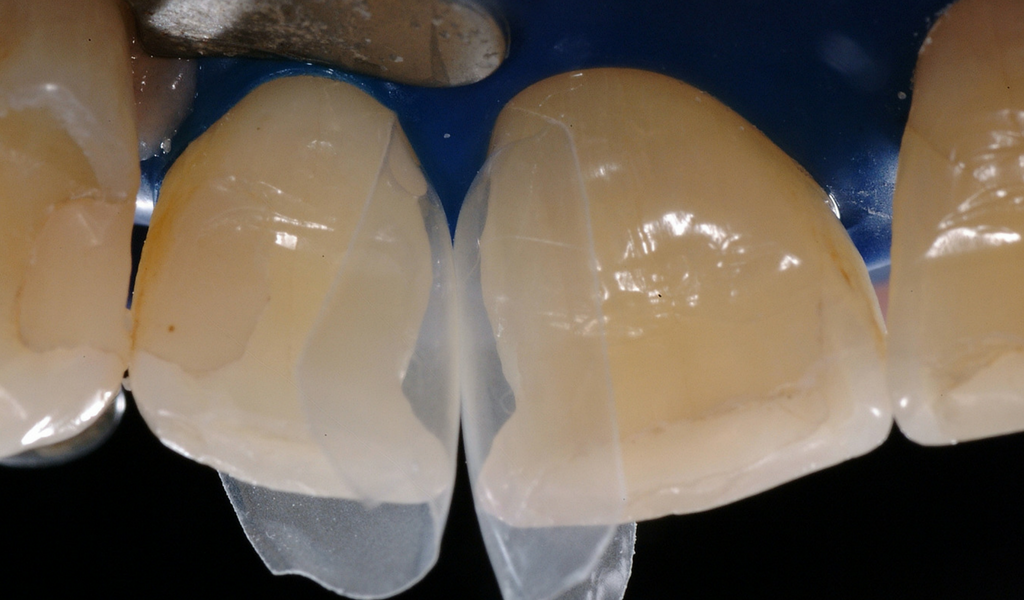
A rubber dam was placed, and the affected area was prepared with with modern, non-retentive composite preparations with infinity edge margins.
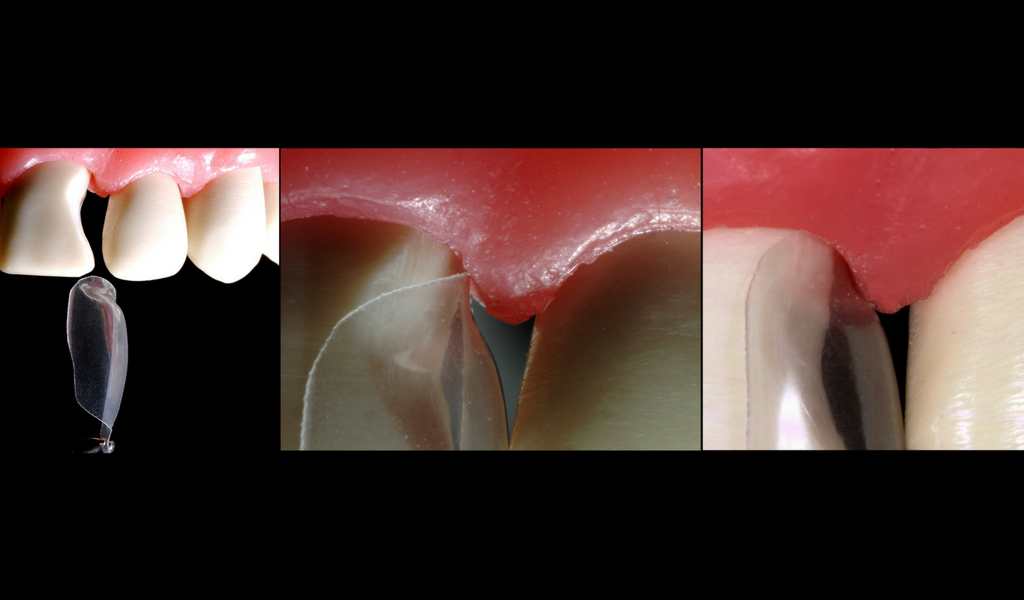
Many traditional diastema treatments achieve closure with composite (or porcelain) that reaches mesiodistally; on top of the gingiva, or in midtooh. The key in this new technique, is to provide aggressive cervical curvature that begins subgingivally.
This is where the Bioclear Matrix System comes in. When used, it allows for the smooth yet aggressive cervical structure which transitions rapidly to an anatomic root shape.
The direct composite architecture achieved with the Bioclear Matrix System is conducive to papilla regeneration, which is down to inherent features:
- No traditional wedge: By forgoing the traditional wedge, clinicians can avoid a flat cervical shape which lacks the pressure needed to regenerate papillae. Instead, the papilla can be used as a wedging force. As the matrix slides into the sulcus, the papilla is engaged; the papilla stabilises the matrix, while the matrix compresses the papilla.
- Anatomic shape: The complete anatomic shape permits the clinician to simply remove the matrix after photo polymerization, with little to no interproximal finishing.
These inherent features are in sharp contrast to the outdated notion that prosthetic and restorative embrasures should be flat. In fact, when the finish is smooth, with a lack of gingival ledge, tissue health can be good - even with very round embrasure form.
Black Triangle Treatment: Step 2
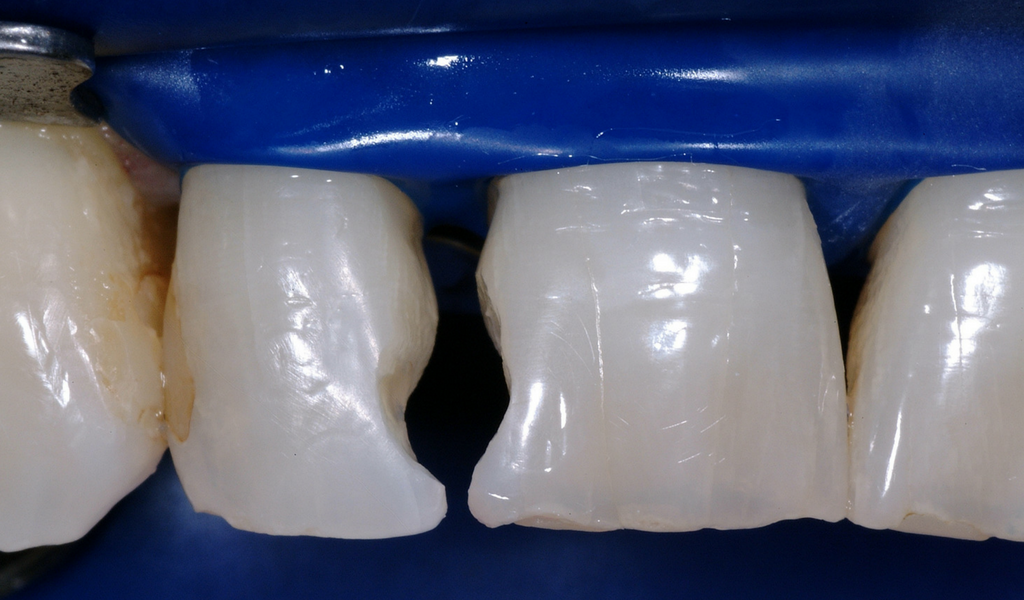
The diastema closure matrices were fully seated, and the gingival edge of the matrix was 3mm sub-gingival. A small drop of water was used to lubricate their insertion - this method rarely causes bleeding as the pre-curved shape does not exit the sulcus.
Black Triangle Treatment: Step 3
The teeth were etched using the total etch technique, as this is deemed a robust method when bonding to large enamel areas. This is especially true for uncut enamel.
Please note, there is no need to stabilise these matrices as they are self-stabilising. However, a metal matrix can be used if needed. This should be hand burnished and annealed over an alcohol torch.
After placing bonding agent (this was not light cured), an initial small increment of flowable composite was carefully injected to fill the crucial cervical area. This was then light cured.
Flowable composite was used in the first increment, rather than paste composite. This is because paste composite presents problems when trying to place in the ‘claustrophobic’ areas, making it difficult to fill the space completely, without disturbing the matrices.

Advanced magnification is paramount for this step, and has become an expected part of this method if you want to achieve optimal soft tissue response.
Black Triangle Treatment: Step 4
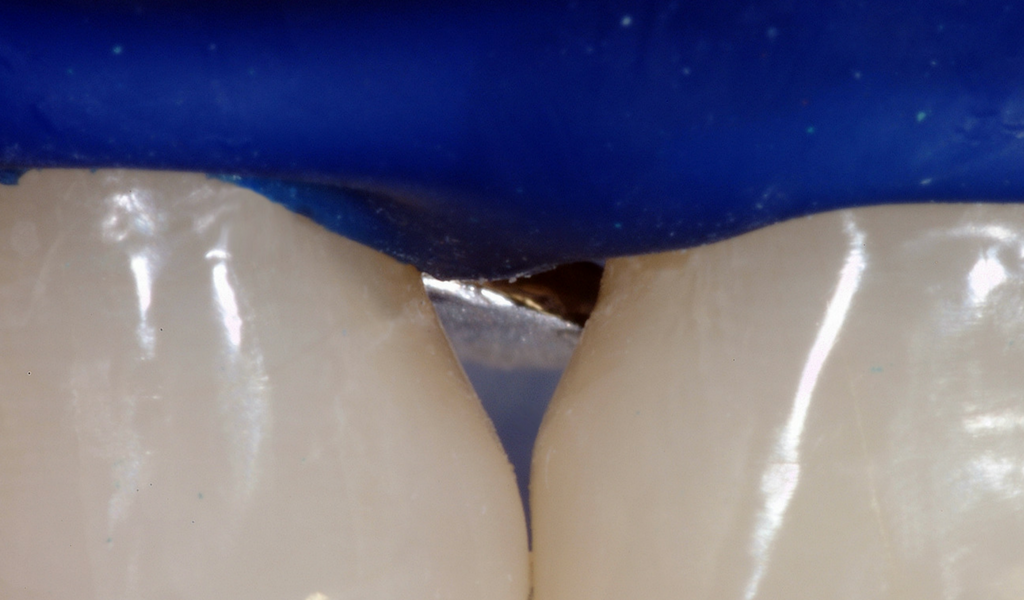
After the initial increment of flowable composite was placed and cured, a silicone Interproximator was inserted to gain tooth separation. An Interproximator, or alternatively a traditional wedge, is necessary in order to compensate for the thickness of the Mylar.
In this instance, the Interproximator was used as it can reduce patient discomfort that is often caused when the traditional wedge presses the palatal tissue.
If neither of these are placed at this stage in the treatment, there is a risk that the contact may be open when the matrices are removed…
Black Triangle Treatment: Step 5
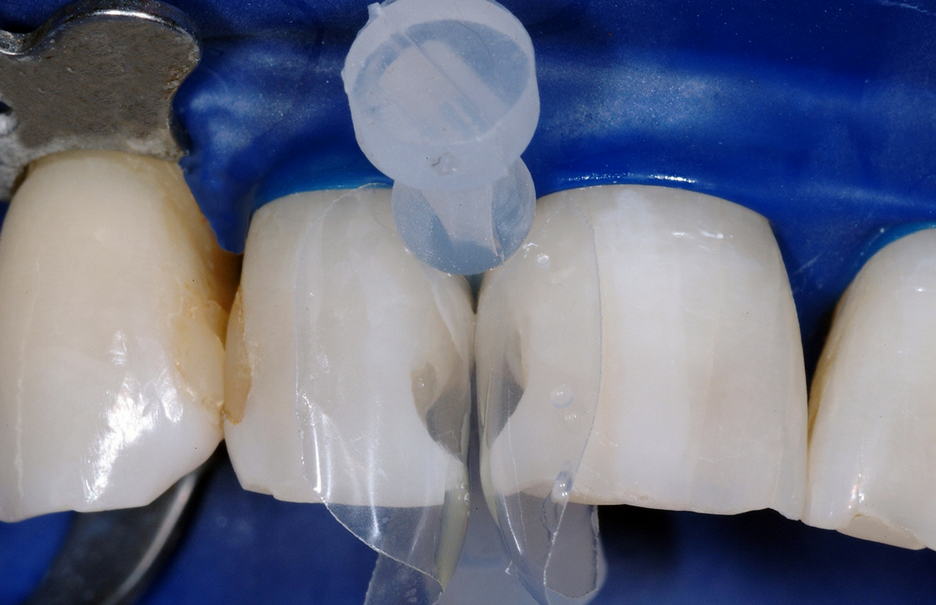
The matrices were removed, revealing a smooth and extremely durable surface. The patient was extremely happy with the results of the treatment.

Accessible Methods For Papilla Regeneration
Natural interproximal embrasures are constructed with a wide range of cervical shapes and varying root proximities. Clinicians are able to create convenient, interproximal shapes if the restorations are smooth and without a sharp marginal ledge.
Restoratively driven papilla regeneration should become a viable option for all restorative dentists.
Our free guide addresses the problem of unnecessarily aggressive restorative treatments, presenting a range of conservative solutions for treating black triangles, Class II restorations and peg laterals, as well as closing diastemas.
*This case was originally presented by Dr David Clark.